Male Genitalia and Rectal System
Assessment – Male Genitalia and Rectal System
Inspection
- Inspect the external male genitalia, noting colour, lesions, drainage, edema, and hair distribution; if assessing an adolescent, assess pubertal development using Tanner stages.
- Inspect the penis on the ventral, lateral and dorsal sides; note if the patient is circumcised; if the patient is not circumcised, assess for phimosis (ability to retract the foreskin or prepuce). Note the location of the urethral opening; assess the pattern of pubic hair distribution; assess the skin for irritation, erythema, and pubic lice.
- Lift the scrotum to inspect the front and back, noting skin colour contour; next, compare the scrotal sac bilaterally, noting contour.
- Inspect the urinary meatus and note any discharge, lesions, or hypospadias.
- With the patient standing and the provider sitting facing the patient, inspect the inguinal regions and genitalia for bulging and asymmetry.
Palpation
- Palpate the inguinal nodes, noting size, consistency, and tenderness.
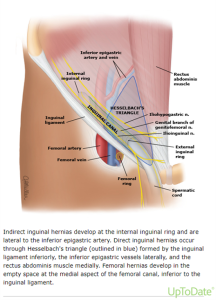
- Assess the groin area for an inguinal hernia; if suspected, ask the patient to cough to visualize better or palpate the inguinal hernia.
- Palpate the penis for tenderness, induration, and lesions.
- Palpate the scrotum for masses, lumps, veins, and edema.
- Palpate the testes for size, shape, consistency, tenderness, masses, and nodules.
- Palpate the epididymides, spermatic cord, and vas deferens for tenderness, thickening, and masses.
- Palpate internal and external inguinal rings.
- Palpate femoral triangle (assess femoral pulse, palpate for femoral hernia).
Advanced Techniques
Assess for Inguinal Hernia
Prostate Exam
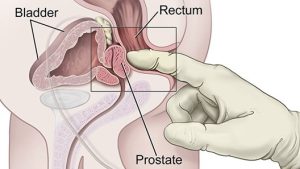
- With the clinical examination table flat, ask the patient to lie in the left lateral position with their knees bent towards their chest, or ask the patient to lie flat on their stomach with the left knee pointed toward the chest.
- Lubricate the examining finger and insert it into the anal canal at the 6 o’clock position. Follow the sacral curve, the prostate will be palpated anteriorly.
- In males, palpate the prostate gland anteriorly and assess the size, symmetry, and texture of the gland. The gland should produce approximately one centimetre into the rectum’s lumen and be about 3.5 cm wide at its average size. The normal prostate has a smooth surface, is rubbery and firm, and has a palpable sulcus between the left and right lobes. There should not be any nodules or tenderness in it.
Examination Checklist
PRINTABLE 10.0
Documenting Assessment Findings
A routine exam should document the following: the status of circumcision, the absence of penile discharge or lesions, the absence of scrotal edema or discoloration, bilaterally descended testes with smooth surfaces and no masses, non-tender epididymis, and the absence of inguinal or femoral hernias. The examiner should also note that the urethral meatus is appropriately placed, and that uncircumcised males’ prepuces can be easily retracted (Endo consult, n.d.).

