Abdominal System
Assessment – Abdominal System
Optimal assessment occurs with the patient lying flat on a semi-firm surface with the abdomen fully visible. All four assessment domains (inspection, auscultation, percussion, and palpation) are required.
Inspection
The patient lies flat with arms placed at the sides. The abdomen is visually assessed for:
- Symmetry – does each quadrant appear similar?
- Contour – is the abdomen flat, protuberant, or scaphoid (concave)?
- Skin – observe for any scars, striae, rashes, lesions, dilated veins
- Umbilicus – look for inflammation, bulges
- Peristalsis – are there any visible waves of motion over the intestines?
- Aortic Pulsations – are there any visible pulsations on the abdomen?
Auscultation
Auscultation must be performed before palpation. The following characteristics are assessed through auscultation:
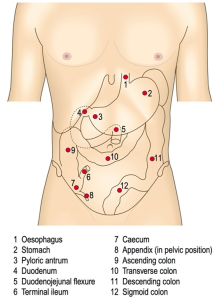
- Bowel sounds are auscultated in all four quadrants noting frequency and character (Listen along the midclavicular lines in the four quadrants, pausing between locations).
- Auscultate for bruits (vascular sounds) over the aorta, renal, iliac, and femoral arteries
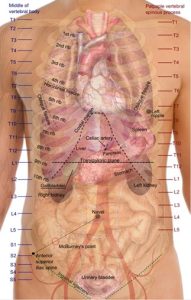
- Aorta: slightly below the xiphoid process midline with the umbilicus
- Renal arteries: go slightly down to the right and left at the aortic site
- Iliac arteries: go a few inches down from the belly button at the right and left sides to listen
- Femoral arteries: found in the right and left groin.
- Listen for venous hums or friction rubs over the liver and spleen.
Percussion
Technique
Middle finger is hyperextended, and the distal interphalangeal joint [DIP] is pressed on the skin surface. The middle finger of the striking hand briskly strikes the DIP joint.
- Percuss generally for distribution of tympany and dullness (Percuss in all nine areas and try to distinguish between dullness over the liver and tympany over the splenic flexure).
- Measure the span of liver dullness at the right midclavicular line (Percuss downward starting just under the breast along the midclavicular line until dullness is heard, then percuss from the level of the umbilicus upward until dullness is heard and measure the span of dullness).
- Assess for splenomegaly (Splenic percussion sign: Percuss at the anterior axillary line at the lowest interspace and ask the patient to take a deep breath while continuing to percuss).
Palpation
Position the patient appropriately with the knees bent, head supported, and arms at the side.
- Use light palpation for tenderness, guarding, or superficial masses (This should be very superficial; use the hand in a horizontal plane and slide the hand or barely lift the hand to the next location to palpate, moving slowly in four or nine areas.)
- Use deep palpation for tenderness and masses (Palpate much deeper; depress skin ~2–3”.)
- Palpate for rebound tenderness to assess for peritoneal inflammation (Press down slowly in the area of tenderness, then release quickly.)
- Describe palpable masses in terms of their location, size, shape, consistency, tenderness, pulsation, and mobility
- Palpate liver edge, spleen, and kidneys for enlargement and tenderness
- Liver: Place left hand posteriorly around the 11th and 12th ribs and press up toward the ceiling. Palpate downward and upward [not in a scooping fashion] with the right hand, starting from the level of the umbilicus until the lowest rib. Ask the patient to take a deep breath and try to feel the liver’s edge as it moves under the fingertips. The hooking technique may be helpful in patients who are obese.
- Spleen: Reach over and use your left hand to press the left lower rib cage upward while using your right hand, starting well below the left costal margin to press upward. Ask the patient to take a deep breath and feel for the spleen’s edge (not usually palpable unless enlarged).
- Kidneys: Palpate along the midclavicular line at the level of the liver edge or costal margin bilaterally.
- Palpate for aortic width: Palpate deep enough with fingertips trapping each side of the aorta, just left of midline.
Advanced Techniques
- Costovertebral angle (CVA) tenderness: Use fist percussion to strike firmly against the hand lying over the CVA bilaterally.
- Ascites: Test for shifting dullness or fluid wave by percussing outward in a stellate pattern from the central area of the tympany and map the border between tympany and dullness. Repeat steps with the patient lying on the side; if no ascites, tympany and dullness stay constant. Ask the patient to press the edges of their hands down the midline. Tap one side of the abdomen, feeling for the wave to hit the opposite hand on the opposite side.
- Appendicitis: Assess for Rovsing sign [right-sided pain during left-sided pressure], psoas sign [pain during resisted right hip flexion or passive right hip extension], and obturator sign (pain with right hip flexion and internal rotation); ask patient to cough.
- Cholecystitis: Assess for Murphy sign by palpating the liver edge and asking the patient to take a deep breath. Watch for a sharp pain that stops inspiration.
Video
VIDEO 8.0
Abdominal Assessment Video
Examination Checklist
Printable 8.0
Printable 8.1
Documentation of Assessment Findings
Documentation of normal or expected findings
The abdomen is soft, flat, and symmetric. There are no visible pulsations or peristalsis, the abdominal surface is absent of scars, rashes, lesions, and striae. There are no visible hernias; bowel sounds are normoactive and present in all four quadrants. No bruit noted over renal, iliac, or femoral arteries; the aortic width was measured at 2 cm. There is no tenderness or masses noted on palpation. Patient denies nausea, vomiting, epigastric discomfort, bloating, constipation, diarrhea, urinary pain, urgency, or frequency. Patient denies appetite changes, food intolerances, dysphagia, or personal or family history of abdominal disorders.
Documentation of abnormal findings
The abdomen is firm and mildly distended, bowel sounds are hyperactive and high-pitched, patient reports intermittent, sharp, colicky, 7/10 pain to the left lower quadrant. There is tenderness on deep palpation to the left upper and lower quadrants; no masses are appreciated. Patient reports a three-day history of pain with intermittent nausea without emesis; abdomen feels full and bloated; patient can pass rectal flatulence, reports last bowel movement yesterday and notes that it was small and constipated. The patient reports a three-day history of low-grade fever and chills.

