Cardiovascular and Peripheral Vascular System
Anatomy and Physiology Review – Cardiovascular and Peripheral Vascular System
Peripheral Vascular System
Arterial
Arteries are responsible for transporting blood away from the heart to the rest of the body tissues. Arteries contain three concentric layers of tissue: the intima, the media, and the adventitia. The intima is the innermost layer; it is here that atherosclerotic plaque formation begins. The media comprises smooth muscle cells with elastic properties to accommodate blood pressure and flow. The adventitia is the outermost layer of the artery, consisting of connective tissue (Bickley, 2021; Thompson, 2018).
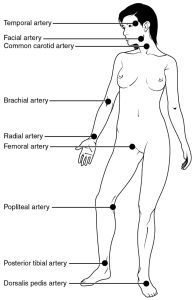
Arterial pulses are palpable throughout the body :
Venous
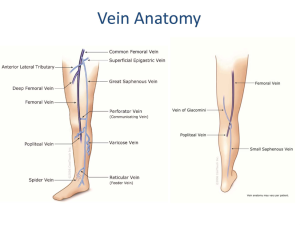
The heart’s pumping action propels blood out of the heart via the arterial system by moving from an area of high pressure to low pressure. Both arteries and veins have the same three distinct tissue layers: the intima, media, and adventitia. Unlike arteries, veins are thin-walled and stretchy; as a result, they can hold up to two-thirds of circulating blood flow in the human body.
Veins from the arms, upper trunk, and head and neck drain into the superior vena cava, veins from the abdominal wall, liver, lower trunk, and legs drain into the inferior vena cava. Veins of the lower extremities include deep, superficial, and perforating veins. Due to their weaker wall structure leg veins are susceptible to irregular dilatation, compression, ulceration, and invasion by tumours (Bickley, 2021, chp. 17).
The venous system returns blood to the heart and must, therefore, have a higher pressure gradient than the heart’s atria. Two factors allow venous pressure to remain higher than the pressure in the atria.
- During diastole, the pressure in the atria is very low as the atria are relaxed
- Two physiologic pumps (skeletal muscle and respiratory pumps) counteract gravity and help the lower pressured veins propel blood back to the heart with the help of skeletal muscle contraction and pressure changes in the thorax.
-
- The blood is compressed, and the pressure is increased near a vein by the contraction of the skeletal muscles. As a result, blood is pushed closer to the heart, where venous pressure is lower. When we exhale, pressure in the thorax is reduced to lower than that of the abdominal veins, causing blood to flow along its pressure gradient from veins outside the thorax into the thoracic region, where pressure is now lower, which promotes the return of blood from the thoracic veins to the atria. As the thoracic cavity’s air pressure rises during exhalation, pressure in the thoracic veins also rises, accelerating blood flow into the heart (Bickley, 2021; Thompson, 2018).
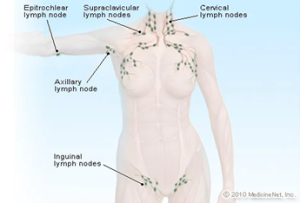
Lymphatics
The lymphatic system is a vascular network that drains lymph fluid from body tissues and returns it to venous circulation for eventual return to the heart. Different body parts drain lymphatic fluid into ducts that drain into the right and left subclavian veins (Betts et al., 2022).
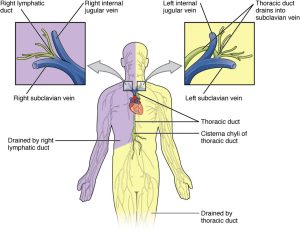
This fluid is filtered through lymph nodes that are present throughout the body. In addition to vascular functions, the lymphatic system plays an essential role in immune function by digesting cellular debris and bacteria and producing antibodies. There are superficial and deep lymph nodes; only the superficial nodes are palpable on physical exam (Thompson, 2018).
Cardiovascular System
Structurally, the heart is comprised of cardiac chambers and heart valves. Physiologically, the cardiac system includes cardiac cycle phases and a complex electrical conduction system. The heart is a two-sided pump that moves blood from the right side of the heart (right atria and right ventricle) to the pulmonary system, where it picks up oxygen. The blood is then returned to the left side of the heart (left atria and left ventricle) to be pumped to the whole body (Betts et al., 2022).
Cardiac Anatomy
The Heart
The heart is a hollow fist-sized muscular organ that contracts and relaxes. When the heart muscle contracts, also known as systole, it pushes blood out to the rest of the body; when the muscle relaxes, also known as diastole, the heart fills with blood).
The base of the heart is the widest portion of the organ (top of the heart), and the apex (bottom of the heart) is the narrowest. The posterior portion of the heart rests on the diaphragm; the precordium is the anterior chest wall that overlays the area of the heart; a muscular septum separates the left and right sides of the heart into two halves. The heart has a dedicated vascular system comprised of the aorta, arteries, arterioles, capillaries, and veins, with blood supplied mainly by the right and left coronary arteries.
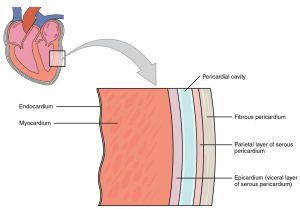
The membrane that directly surrounds the heart and defines the pericardial cavity is called the pericardium or pericardial sac. This membrane consists of three layers: the fibrous pericardium, the parietal layer of the serous pericardium, and the epicardium (visceral layer of the pericardium), plus the pericardial cavity. The heart wall also consists of three layers: the most superficial layer is called the epicardium, as mentioned previously, the middle layer is the myocardium, and the deepest layer is called the endocardium. The pericardial fluid in the cavity protects and lubricates the heart during contraction and relaxation (Betts et al., 2022).
Cardiac Chambers
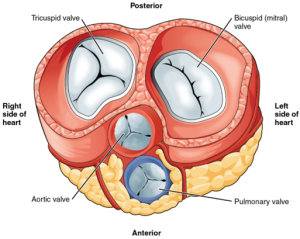
The heart has four chambers and four valves. The atrioventricular septum separates the two atrial chambers, and the interventricular septum separates the two ventricular chambers. Blood flows through each chamber through small openings called valves.
Heart Valves
Four heart valves permit blood flow through the heart in a forward motion. There are two atrioventricular valves; the tricuspid valve separates the right atria from the right ventricle, and the mitral valve separates the left atria from the left ventricle. Two semilunar valves separate the ventricles from the pulmonary artery and the aorta. The pulmonic valve separates the right ventricle from the pulmonary artery, and the aortic valve separates the left ventricle from the aorta (Betts et al., 2022).
Heart Sounds
Normal heart sounds
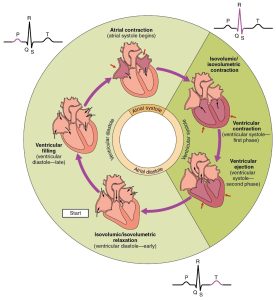
As the heart contracts and relaxes, a rapid deceleration of blood flow causes the heart valves to close at the beginning and end of each contraction. Closure of the atrioventricular and semilunar valves creates the first (S1) and second (S2) heart sounds when auscultating the heart with a stethoscope. The first sound reflects the closure of the atrioventricular valves (mitral and tricuspid), and the second heart sound is produced by the closure of the semilunar valves (pulmonic and aortic). The interval between S1 and S2 is the systole period, and the space between S2 and the start of the next S1 sound is the diastole period (Betts et al., 2022; Bickley, 2021).
Extra heart sounds
Extra heart sounds are heard in different parts of the diastolic phase of the cardiac cycle. Diastole is the portion of the cardiac cycle when the heart muscle is relaxed and the heart chambers are filling with blood (Betts et al., 2018; Thompson, 2018).
a) S3 heart sounds occur in early diastole and are produced when much blood rushes into the ventricles (lub-dub-ta). S3 sounds can indicate fluid overload, as occurs in congestive heart failure. This can be a normal finding in a pregnant female due to the extra blood circulating during pregnancy (Betts et al., 2022).
b) S4 heart sounds occur in late diastole (ta-lub-dub) and are related to stiff ventricles that are not relaxing as quickly as they should be. S4 heart sounds are thus typically related to pressure overload or severe hypertension (Bickley, 2021).
c) Heart Murmurs – the audible sound of a heart murmur is created as a result of turbulent or rough blood flow through the heart. These murmurs are generally graded on a scale of one to six, with one being a slight murmur and six signifying a significant murmur.
| Grade 1 | just audible with a good stethoscope in a quiet room |
|---|---|
| Grade 2 | quiet but readily audible with a stethoscope |
| Grade 3 | easily heard with a stethoscope |
| Grade 4 | a loud, obvious murmur with a palpable thrill |
| Grade 5 | very loud, heard only over the pericardium but elsewhere in the body |
| Grade 6 | heard with stethoscope off the chest |
Heart murmurs in children can be non-pathologic or “innocent” and reflect normal blood flow through thin heart walls. Pathologic murmurs are caused by age-related changes in the heart, underlying heart disease, or structural disease of the heart valves (Bickley, 2021).
For more information on the assessment of extra heart sounds and corresponding audio files, please click on the following links:
Cardiac Physiology
Cardiac physiology is one of the most important concepts in healthcare. The amazing ability of the heart to adapt and interact with every other body system is truly remarkable. By regulating heart rate (the number of beats of the heart per minute), stroke volume (the volume of blood moved out of the left ventricle at the end of systole), preload (the volume at which the heart is most filled with blood at the end of diastole; this value is equal to end-diastolic volume (EDV), afterload (the pressure the left ventricle must overcome to eject blood into the Aorta during systole), diastole (the phase of the cardiac cycle that consists of relaxation and filling of the ventricles with blood) and systole (the phase of the cardiac cycle that consists of contraction of the ventricles and ejection of the blood), the heart can maintain homeostasis (stability) in a very complex system (Oberman & Bhardwaj, 2022).
Phases of the Cardiac Cycle
The cardiac cycle begins with one heartbeat and ends with the start of another heartbeat. The atria and ventricles contract and relax to propel blood through the body. Each cycle consists of diastole (cardiac muscle relaxation) and systole (cardiac muscle contraction). When the atria are relaxing, the ventricles are contracting and vice versa (Betts et al., 2022).
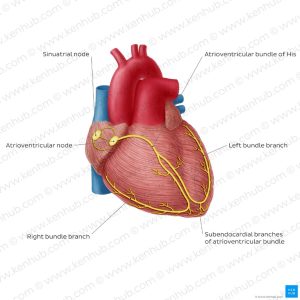
Conduction System of the Heart
The heart’s conduction system comprises specialized cardiac muscle cells (myocytes) that transmit electrical impulses that produce the coordinated muscle contractions of each cardiac cycle.
The physiological pacemaker of the heart is the sinoatrial node (SA node) because it is the primary impulse initiator and regulator of a healthy heart. The atrioventricular node (AV node) conducts electrical impulses from the SA node to the heart ventricles. This is achieved via atrioventricular bundles (bundle of His) and the Purkinje fibres in the ventricle walls (Assadi & Motabar, 2018).