Module 2 Guidelines for Completing the Medical Certificate of Death
Cause of Death- Section 7
7. Ensure this section is completed as accurately and completely as possible.
Guidelines for Determining Cause of Death
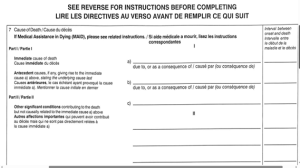
This section contains two parts, Part I is designed to record the sequence of conditions causing death in an ascending casual order with one cause recorded per line, and Part II is designed to record any significant contributing conditions. The cause of death reported is to be the best opinion/reasonable determination of the individual completing it. Your duty is to indicate a cause of death as accurately as possible recognizing that medicine is not an exact science, and an exact cause of death is sometimes elusive. The cause must consist of a diagnostic entity which is a term used to describe a disease or other morbid condition (Office of the Registrar General, 2010). The cause of death must only meet the test of “being more likely than not” (Saskatchewan Coroners Service, nd). It is sometimes easiest to consider the conditions leading up to the death in a bottom to top fashion with the immediate cause being the top.
Important Definitions
Underlying Cause of Death (Part I)
The disease that initiated the chain of events that led directly to the death. This is considered to be what started it all, the first and oldest condition and must have caused all of the conditions on the lines above it (reported on line C in Part I of the Medical Certificate of Death).
Intermediate (Antecedent) Cause of Death (Part I)
For some deaths, the sequence of disease involves conditions that occur at a time between the underlying cause and immediate cause. This is considered to be an event older than the condition listed on line A and newer than the condition listed on line C (recorded on line B in Part I of the Medical Certificate of Death).
Immediate Cause of Death (Part I)
The final disease or complication resulting from the underlying cause of death that directly caused death. This is considered to be the most recent condition that caused the death (recorded on line A in Part I of the Medical Certificate of Death).
The terms cardiac arrhythmia, asystole, shock, exsanguination, respiratory failure, or cardiac arrest should never be used as an immediate cause of death (line A Part I) unless it is accompanied by a specific disease entity (line B or C Part I).
It is not necessary or always required to use all the lines in Part I. The underlying, intermediate, and immediate cause of death are linked in a cause-and-effect relationship from bottom to top.
Other Significant Conditions (Part II)
Pre-existing or co-existing disease(s) that contributed to death but did not result in the underlying cause of death (recorded in Part II of the Medical Certificate of Death).
Interval Between Onset and Death
This section is used to record the time interval between the presumed onset of the condition (not necessarily the date of diagnosis) and the date of death. Intervals should be listed for all conditions in Part I, they are established by the certifier on the basis of available information. In some cases, this interval will have to be estimated and the terms unknown or approximately may be used. This time can be stated in minutes, hours, days, or months or if it is entirely unknown state the interval as unknown. This information is useful in coding diseases and provides a useful check on the accuracy of the reported sequence of conditions (Saskatchewan Coroners Service, nd).
Cause of Death Examples
Example 1
A 70 year old man with documented cardiovascular disease (diagnosed 20 years ago) requiring nitroglycerin was found deceased in bed. There was a history of hypertension and prior ECG showed ventricular hypertrophy. No autopsy was performed, and it is unknown whether he had an acute myocardial infarction or a fatal dysrhythmia without infarction. There is no evidence of injury or foul play.
Medical Certificate of Death:
Part I line C -Atherosclerotic Cardiovascular Disease (an all encompassing term that reflects death caused by cerebrovascular accident, pulmonary embolism, and cardiac death). The interval is listed as 20 years.
Part II- Hypertension
Example 2
A 55 year old woman with long standing hypertension. Over time she developed renal failure (3 years prior to death) ultimately requiring dialysis which became ineffective and she died of severe uremia.
Medical Certificate of Death:
Part I line C- Hypertension. The interval listed is 20 years.
Part I line A- Dialysis dependent renal failure. The interval listed is 3 years.
Example 3
An elderly woman with dementia is bedridden. The dementia was diagnosed 6 years from the date of death and she became bedridden 2 years prior to death. She developed pressure ulcers and within a week of death developed a wound infection with fatal systemic sepsis. She had diabetes.
Medical Certificate of Death:
Part I line C- Dementia. The interval listed is 6 years.
Part I line B- Immobility and bedridden. The interval listed is 2 years.
Part I line A- Systemic bacterial infection from pressure ulcers. The interval listed is 1 week.
Example 4
A person with longstanding alcoholism developed cirrhosis 3 years ago, followed by hepatic encephalopathy. There was also some GI bleeding and pneumonia which complicated management and were thought to have contributed to the death.
Medical Certificate of Death:
Part I line C- Chronic alcoholism. The interval listed is unknown.
Part I line B- Cirrhosis of the Liver. The interval listed is 3 years.
Part I line A- Hepatic encephalopathy. The interval listed is the number of days.
Part II- Gastrointestinal bleeding (listed in Part II as it was thought to have contributed to death and resulted from chronic alcoholism but did not result in chronic alcoholism)
Pneumonia (listed in Part II as it was thought to have contributed to death)
Example 5
An elderly man has small cell lung cancer with metastases to the brain. An autopsy was not performed as death was expected.
Medical Certificate of Death:
Part I line C- Small cell carcinoma of the lung with metastases to the brain. The interval listed is 10 months.
Example 6
A 67 year old male has known coronary artery disease (CAD) diagnosed 15 years ago. At home he had chest pain and goes to the ER, dying before diagnostic tests can be performed.
Medical Certificate of Death:
Part I line C- Coronary Artery Disease. The interval listed is 15 years.
Part I line A- Probable Acute Myocardial Infarction. The interval listed is minutes.
It is acceptable to use the word probable or presumed when certainty about the cause of death is lacking.
Example 7
Shortly after dinner on the day prior to admission to the hospital, a 48-year-old male developed a cramping, epigastric pain, which radiated to his back, followed by nausea and vomiting. The pain was not relieved by
positional changes or antacids. The pain persisted, and 24 hours after its onset, the patient sought medical attention. He had a 10-year history of excessive alcohol consumption and a 2-year history of frequent episodes of similar epigastric pain. The patient denied diarrhea, constipation, hematemesis, or melena. The patient was admitted to the hospital with a diagnosis of an acute exacerbation of chronic pancreatitis. Radiological findings included a duodenal ileus and pancreatic calcification. Serum amylase was elevated. The day after admission, the patient seemed to improve. However, that evening he became disoriented, restless, and hypotensive. Despite intravenous fluids and vasopressors, the patient remained hypotensive and died.
Medical Certificate of Death:
Part I line C- Chronic alcohol abuse. The interval listed is 10 years.
Part 1 line B- Chronic pancreatitis. The interval listed is 2 years.
Part I line A- Acute exacerbation of chronic pancreatitis. The interval listed is 3 days.
Example 8
A 75-year-old male was admitted to the hospital complaining of severe chest pain. He had a 10-year history of arteriosclerotic heart disease with ECG findings of myocardial ischemia and several episodes of congestive
heart failure controlled by digoxin and diuretics. Five months before this admission, the patient was found to be anemic, and to have occult blood in the stool. A barium enema revealed a large polypoid mass in the cecum diagnosed as carcinoma by biopsy. Because of the patient’s cardiac status, he was not considered to be a
surgical candidate. Instead, he was treated with a 5-week course of radiation therapy and periodic packed red blood cell transfusions. He completed this course 3 months before this hospital admission. On this admission the ECG showed an acute anterior wall myocardial infarction. He expired 2 days later.
Medical Certificate of Death:
Part I line B- Atherosclerotic cardiovascular disease. The interval listed is 10 years.
Part I line A- Acute myocardial infarction. The interval listed is 2 years.
Part II- Carcinoma of cecum (listed in Part II as it was thought to have contributed to death)
Congestive heart failure (listed in Part II as it was thought to have contributed to death)
Example 9
A 34-year-old male was admitted to the hospital with severe shortness of breath. He had a 9-month history of unintentional weight loss, night sweats, and diarrhea. The patient had no history of any medical condition
that would cause immunodeficiency. A test for human immunodeficiency virus (HIV) was positive. A lung biopsy was positive for pneumocystis carinii pneumonia (PCP), indicating a diagnosis of acquired immunodeficiency syndrome (AIDS). The patient’s pneumonia responded to therapy, and the patient was discharged. The patient had two additional admissions for PCP. Seventeen months after the patient was first discovered to be HIV positive, he again developed PCP but did not respond to therapy. He died 2 weeks later.
Medical Certificate of Death:
Part I line C- HIV infection. The interval listed is over 17 months.
Part I line B- Acquired immunodeficiency syndrome. The interval listed is 17 months.
Part I line A- Pneumocystis carinii pneumonia. The interval listed is 2 weeks.
It is important to note that AIDS is due to HIV infection, the terms are not synonymous
Example 10
A 75-year-old male had a 10-year history of chronic bronchitis associated with smoking two packs of cigarettes a day for more than 45 years. When seen by his physician approximately 2 years prior to his terminal episode, he had moderately reduced FEV1 and FVC with no response to bronchodilators. During his last year, he required corticosteroids to prevent wheezing and coughing at night; however, he was unable to reduce his smoking to less than one pack of cigarettes per day. When seen 2 months prior to his terminal episode, he had significantly reduced FEV1 and FVC with no response to bronchodilators. He awoke one evening complaining to his wife about coughing and worsening shortness of breath. He was taken to the emergency room where he was found to have an acute exacerbation of obstructive airway disease. He was admitted to the hospital. At the patient’s request, no mechanical ventilation was initiated, and he died 12 hours later in respiratory arrest.
Medical Certificate of Death:
Part 1 line B- Chronic bronchitis. The interval listed is 10 years.
Part 1 line A- Acute exacerbation of obstructive airway disease. The interval listed is 12 hours.
It is important to note that respiratory arrest is a mechanism of death not a cause so it is not listed on the Medical Certificate of Death.
Cause of Death Errors
A nonspecific anatomical process is a complication of an underlying cause of death and may be a macroscopic or microscopic alteration that may have consequences and more than one possible cause (i.e., cirrhosis).
A mechanism of death is a nonspecific functional disturbance that is a complication of an underlying cause of death and may have more than one cause (i.e., hemorrhage).
It is appropriate to include the above in cause of death statements as immediate or intermediate causes of death but must be accompanied by the underlying cause of death.
The most common processes used in error (i.e., alone with no accompanying disease entity):
- Sepsis, congestive heart failure, gastrointestinal hemorrhage, hypoxic brain injury, cirrhosis, pneumonia, renal failure, bowel obstruction, pulmonary edema, abdominal hemorrhage, intracranial hemorrhage.
- Hemorrhage, peritonitis, hepatic encephalopathy, metabolic encephalopathy, cerebrovascular insufficiency, multi organ failure, abscess, acute MI, altered mental status, anemia, arrhythmia, ascites, aspiration, atrial fibrillation, cardiomyopathy, cellulitis, compression fracture, dehydration, dementia, end stage renal or liver disease, failure to thrive, hepatitis, hyperglycemia, hyperkalemia, hypotension, old age, pleural Effusion, pulmonary embolism, respiratory arrest, shock, sudden death, urinary tract infection (Saskatchewan Coroners Service, nd).
Deaths Associated With Aging
There is no uniformly accepted way to document the cause of death in the elderly when the death is natural. Using terms such as old age, infirmity, and advanced age should not be used for convenience. Instead, if there is a specific condition that has a high likelihood of having caused death, that condition should be listed as the underlying cause of death. If an underlying cause of death is elusive (for example the elderly on no medications) the death can be listed as “unspecified natural causes” (Saskatchewan Coroners Service, n.d.).

