Chapter 8: Prevention of Illness
Respiratory Transmission
Fecal-Oral Transmission
Food Poisoning
Direct Contact Transmission
Bodily Fluid Transmission
Vector-Borne Transmission
Universal Precautions to Prevent the Spread of Illness
Children’s Environmental Health
Environmental Exposures and Children’s Vulnerability
Outdoor Air Quality
Indoor Air Quality
Mould
Integrated Pest Management
Chemical Hazards
Plastics in Child Care Settings
Drinking Water
References
Chapter 8: Learning Objectives
By the end of this chapter, you should be able to:
- Describe each of the five ways illness is transmitted.
- Explain how immunization prevents illness.
- Identify standard precautions to prevent illness.
- Discuss practices to protect children from environmental hazards
Introduction
Science and experience tell us that infectious disease, especially gastrointestinal disease, which means vomiting and diarrhea, and respiratory disease, including coughs, colds, sore throats, and runny noses, are increased among children who are cared for in out-of-home group settings. In addition, such children may be at increased risk for certain other infections that may be transmitted by insects or by body fluids. It’s also true that children who are cared for in group out-of-home settings are more likely to experience infectious illnesses that are more severe and more prolonged (although 90% of those infections are mild and self-limited, requiring no special treatment).
But there’s good news, too. Infectious illnesses such as pneumonia and influenza, which together were the leading causes of death among Canadian children in the early 20th century, have declined by 99.7 percent. Common childhood illnesses such as diphtheria, whooping cough, measles, mumps, and rubella are rare except in communities where immunization rates are low, and polio is unheard of in our country today.
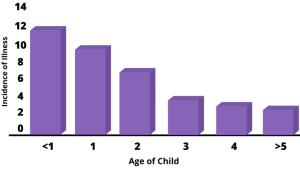
Although younger children are more susceptible to infectious illness because their immune systems are immature, as they grow older, the incidence of infectious disease decreases as their immune systems mature. Furthermore, children who experience more infectious diseases at an early age in group out-of-home care have a decreasing incidence of infectious diseases as they grow older. In fact, they have fewer infectious illnesses in kindergarten than children who were taken care of exclusively at home. Illness also decreases with years of attendance in out-of-home early care and education settings.
There are negative consequences of childhood illness, including:
- It’s unpleasant to be sick (for children or adults who may also become infected).
- Illnesses that are minor in children can be much more serious for adults and pregnant women.
- Some illnesses have severe effects (and can even be life-threatening).
- There may also be additional childcare costs or lost wages for parents/caregivers of children who must be excluded from group care.
- Overuse of antibiotics in an effort to get children well contributes to antibiotic resistance among common bacteria.
To prevent illness we need to understand the different ways illness is spread, how immunizations protect children, and what universal precautions early care and education program staff can take to prevent the spread of illness.
How Illnesses are Transmitted
Bacteria, viruses, fungi, and parasites that cause illness can be transmitted in five ways, including through:
- the respiratory route
- the fecal-oral route
- The direct contact route
- the bodily fluid route (including blood, urine, vomit, and saliva)
- the vector-borne route
Respiratory Transmission
Most respiratory germs stay in the nose, sinuses, mouth and throat, or possibly the middle ear. Upper respiratory illnesses (colds) are the most common and the most likely to be transmitted in early care and education settings.
The more common respiratory illnesses include:
- Sinusitis
- Sore throat
- Common cold
- Recurrent middle ear infection
- Strep throat
- RSV
- Pneumonia
- Bronchitis
Pneumonia and bronchitis are rarely the result of an infection picked up in an early education setting. We also have immunizations for many respiratory diseases that are rarely transmitted in early care and education settings today, including:
- Mumps
- Measles
- Bacterial meningitis
- Chickenpox
- Diphtheria
- Pertussis
- Pneumonia
- Seasonal flu
If we could actually see what comes out of a child’s mouth along with a cough or a sneeze, we might appreciate the respiratory route of infectious disease transmission more.

The germs that are in this contaminated cloud of exhalation can wind up on surfaces and hands and be transmitted to others. Staff and children who are able to are encouraged to cough into their sleeves. Covering your mouth with your hand only transfers these germs to your hand. This will be addressed more in-depth later in the chapter.
Fecal-Oral Transmission
When organisms that live in our intestines get into our mouths they can cause illness. Usually, this happens via someone’s hands, usually our own. Fecal-oral routes diseases include:
- Hepatitis A
- diarrhea
- hand, foot, and mouth disease
- pinworms
- rotavirus
- norovirus
- giardia
- shigella
- cryptosporidiosis
That is why it is so important that everyone wash their hands after using the bathroom, changing diapers, preparing food, and before eating.

Food Poisoning
E. coli and salmonella are two of the germs that you may also have heard mentioned in the news when grocery stores send back fresh vegetables, meat, or poultry. These organisms originate with farm animals themselves and they can cause diarrhea and vomiting if children or staff eat contaminated food. Properly preparing and serving fresh produce, meat, and poultry is essential to prevent food poisoning.
Direct Contact Transmission
Direct contact with another person’s skin (or hair) puts infants and children at risk of illnesses such as:
- cold sores
- conjunctivitis
- pink eye
- impetigo
- lice
- scabies
- ringworm (a fungus, not a worm).
Bodily Fluid Transmission
Bodily fluids, including saliva, urine, vomit, and blood, can cause illness, such as:
- Dental caries (by saliva)
- Cytomegalovirus or CMV (by urine)
- Hepatitis B (preventable by vaccine)
- Hepatitis C (rare in children)
- HIV (no cases of transmission in an early education setting)
Vector-Borne Transmission
A vector is a living thing that can transmit disease. We know, for example, that ticks can transmit Lyme disease and Rocky Mountain spotted fever. Fleas are known to transmit Bubonic plague and typhus. Mosquitoes can infect people with St. Louis encephalitis (SLE), dengue fever, Zika virus, and West Nile disease. Rats and mice can transmit leptospirosis, trichinosis, hantavirus, and bacterial food poisoning. Raccoons can spread raccoon roundworm.
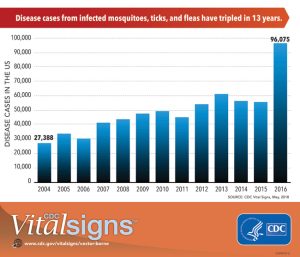
While these illnesses are relatively uncommon, the risk reminds us of the importance of
- utilizing integrated pest management techniques to keep insects and rodents out of buildings (covered later in this chapter)
- using insect repellant specifically recommended for children during outdoor activities
- removing standing water in which mosquitoes can lay their eggs
- checking for and removing ticks (addressed in Figure 4.10) in centers when children come back in after playing in or near heavily wooded areas[4]
The video below explains how disease spreads and how we can slow it down with the “Swiss Cheese” model.
Time: 12:42
Link: https://www.youtube.com/watch?v=1QLgXzyXOH0&t=762s
Transcript: how-does-disease-spread-quick-learn
Source: Centers for Disease Control and Prevention (CDC). CDC Science Ambassador Fellowship—CDC NERD Academy, Atlanta, GA: U.S. Department of Health and Human Services, CDC; 2022. Available at: www.cdc.gov/scienceambassador/nerdacademy. [5]
Pause to Reflect
| Why is it important to understand how illnesses and diseases are spread? |
Immunizations
Prevention of infectious diseases starts with immunizations (or vaccines). Immunizations are considered the number one public health intervention of the 20th century and one of the top 10 interventions of the first decade of the 21st century.[6]
On-time vaccination throughout childhood is essential because it helps provide immunity before children are exposed to potentially life-threatening diseases. Vaccines are tested to ensure that they are safe and effective for children to receive at the recommended ages.[7] See Figure 8.6 for the current schedule of immunizations.
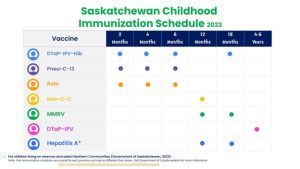
The current schedule of vaccines (see Figure 8.6) protects children from the illnesses listed in Table 8.1)
Table 8.1 – Vaccine-Preventable Diseases.[8]
| Disease | Vaccine | Disease Spread By | Disease Symptoms | Disease Complications |
| Chick-pox | Varicella vaccine protects against chickpox | Air, direct contact
|
Rash, tiredness, headache, fever
|
Infected blisters, bleeding disorders, encephalitis (brain
swelling), pneumonia (infection in the lungs) |
| Diphtheria | DtaP* vaccine protects against diphtheria | Air, direct contact
|
Sore throat, mild fever, weakness, swollen
glands in neck |
Swelling Of the heart muscle, heart failure, coma, Paralysis, death |
| HiB | Hib vaccine protects against Haemophilus
Influenza type b |
Air, direct contact
|
May be no symptoms unless bacteria
enter the blood
|
Meningitis (infection of the covering around the brain
and spinal cord), intellectual disability. epiglottitis (life-threatening infection that can block the windpipe And lead to serious breathing problems), pneumonia (infection in the lungs), death
|
| Hepatitis A | HepA vaccine protects against hepatitis A. | Direct contact, contaminated
food or water
|
May be no symptoms – fever, stomach pain,
loss of appetite. Fatigue, vomiting, jaundice (yellowing of skin and eyes). dark urine |
Liver failure. arthralgia (joint pain), kidney, pancreatic,
and blood disorders
|
| Hepatitis B | HepB vaccine protects against hepatitis B. | Contact With
body fluids
|
May be no symptoms fever, headache,
weakness, vomiting, jaundice (yellowing of skin and eyes), joint pain
|
Chronic liver infection, liver failure, liver cancer
|
| Influenza (Flu) | Flu vaccine protects against influenza.
|
Air, direct contact
|
Fever, muscle pain, sore throat, cough,
extreme fatigue
|
Pneumonia (infection in the lungs)
|
| Measles | MMR* vaccine protects against measles.
|
Air, direct contact
|
Rash, fever, tough, runny nose, pinkeye
|
Encephalitis (brain swelling), pneumonia (infection in
the lungs). death
|
| Mumps | MMR* vaccine protects against mumps.
|
Air, direct contact
|
Swollen salivary glands (under the jaw), fever,
headache, tiredness, muscle pain |
Meningitis (infection of the covering around the brain
and spinal cord) , encephalitis (brain swelling), inflammation Of testes or ovaries, deafness
|
| Pertussis
|
DTap* vaccine protects against pertussis
(whooping cough).
|
Air, direct contact
|
Severe cough, runny nose, apnea (a pause in
breathing in infants) |
Pneumonia (infection in the lungs), death
|
| Polio | IPV vaccine protects against polio.
|
Air. direct contact, through
the mouth
|
May be no symptoms, sore throat, fever,
nausea. headache
|
Paralysis, death
|
| Pneumococcal
|
POII 3 vaccine protects against pneumococcus. | Air, direct contact
|
May be no symptoms -. pneumonia (infection
in the lungs)
|
Bacteremia (blood infection), meningitis (infection of
the covering around the brain and spinal cord). death
|
| Rotavirus | RV vaccine protects against rotavirus.
|
Through the mouth | Diarrhea, fever, vomiting
|
Severe diarrhea, dehydration
|
| Rubella | MMR* vaccine protects against rubella.
|
Air, direct contact
|
Children infected with rubella virus sometimes
have a rash, fever. swollen nodes |
Very serious in pregnant women—can lead to miscarriages, stillbirth, premature delivery, birth defects
|
| Tetanus | DTap* vaccine protects against tetanus.
|
Exposure through cuts in skin
|
Stiffness in neck and muscles,
difficulty swallowing, muscle spasms, fever |
Broken bones, breathing difficulty, death
|
How Vaccines Work
The immune system helps the human body fight germs by producing substances to combat them. Once it does, the immune system “remembers” the germ and can fight it again. Vaccines contain germs that have been killed or weakened. When given to a healthy person, the vaccine triggers the immune system to respond and thus build immunity.
Before vaccines, people became immune only by actually getting a disease and surviving it. Immunizations are an easier and less risky way to become immune.
Vaccines are the best defence we have against serious, preventable, and sometimes deadly contagious diseases. Vaccines are some of the safest medical products available, but like any other medical product, there may be risks. Accurate information about the value of vaccines as well as their possible side effects helps people to make informed decisions about vaccination.

Potential Side Effects
Vaccines, like all medical products, may cause side effects in some people. Most of these side effects are minor, such as redness or swelling at the injection site. Read further to learn about the possible side effects of vaccines.
Any vaccine can cause side effects. For the most part, these are minor (for example, a sore arm or low-grade fever) and go away within a few days.[9] Serious side effects after vaccination, such as severe allergic reactions, are very rare.[10]
Remember, vaccines are continually monitored for safety, and like any medication, vaccines can cause side effects. However, a decision not to immunize a child also involves risk and could put the child and others who come into contact with him or her at risk of contracting a potentially deadly disease.
How Well Do Vaccines Work?
Vaccines work really well. No medicine is perfect, of course, but most childhood vaccines produce immunity about 90–100% of the time.
What about the argument made by some people that vaccines don’t work that well and that diseases would be going away on their own because of better hygiene or sanitation, even if there were no vaccines?
That simply isn’t true. Certainly, better hygiene and sanitation can help prevent the spread of disease, but the germs that cause disease will still be around, and as long as they are they will continue to make people sick.

In Canada Vaccines go through many stages of development and testing, to ensure their safety to human beings before they are made available to the public. They continue to go through ongoing monitoring and review after they are approved and Canadians have access to them. Figure 8.8 demonstrates the development and approval process for all vaccines. Click on the image for more information.
If you look at the history of any vaccine-preventable disease, you will virtually always see that the number of cases of disease starts to drop when a vaccine is licensed. Vaccines are the most effective tool we have to prevent infectious diseases.
Opposition to Vaccines
In 2010, a pertussis (whooping cough) outbreak in California sickened 9,143 people and resulted in 10 infant deaths: the worst outbreak in 63 years (Centers for Disease Control 2011b). Researchers suspect that the primary cause of the outbreak was the waning strength of pertussis vaccines in older children, and they recommended a booster vaccination for 11–12-year-olds and pregnant women (Zacharyczuk 2011). Pertussis is most serious for babies; one in five needs to be hospitalized, and since they are too young for the vaccine themselves, it is crucial that people around them be immunized (Centers for Disease Control 2011b). Several states, including California, have been requiring the pertussis booster for older children in recent years with the hope of staving off another outbreak.
But what about people who do not want their children to have this vaccine or any other? That question is at the heart of a debate that has been simmering for years. Vaccines are biological preparations that improve immunity against a certain disease. Vaccines have contributed to the eradication and weakening of numerous infectious diseases, including smallpox, polio, mumps, chickenpox, and meningitis.

However, many people express concern about the potential negative side effects of vaccines. These concerns range from fears about overloading the child’s immune system to controversial reports about the devastating side effects of the vaccines.[12]
Although children continue to get several vaccines up to their second birthday, these vaccines do not overload the immune system. Every day, an infant’s healthy immune system successfully fights off thousands of antigens – the parts of germs that cause their immune system to respond. Even if your child receives several vaccines in one day, vaccines contain only a tiny amount of antigens compared to the antigens your baby encounters every day.
This is the case even if your child receives combination vaccines. Combination vaccines take two or more vaccines that could be given individually and put them into one shot. Children get the same protection as they do from individual vaccines given separately—but with fewer shots.[13]
One misapprehension is that the vaccine itself might cause the disease it is supposed to be immunizing against.[14] Vaccines help develop immunity by imitating an infection, but this “imitation” infection does not cause illness. Instead, it causes the immune system to develop the same response as it does to a real infection so the body can recognize and fight the vaccine-preventable disease in the future. Sometimes, after getting a vaccine, the imitation infection can cause minor symptoms, such as fever. Such minor symptoms are normal and should be expected as the body builds immunity.[15]
Another commonly circulated concern is that vaccinations, specifically the MMR vaccine (MMR stands for measles, mumps, and rubella), are linked to autism. The autism connection has been particularly controversial. In 1998, a British physician named Andrew Wakefield published a study in Great Britain’s Lancet magazine that linked the MMR vaccine to autism. The report received a lot of media attention, resulting in British immunization rates decreasing from 91 percent in 1997 to almost 80 percent by 2003, accompanied by a subsequent rise in measles cases (Devlin 2008). A prolonged investigation by the British Medical Journal proved that not only was the link in the study nonexistent but that Dr. Wakefield had falsified data in order to support his claims (CNN 2011). Dr. Wakefield was discredited and stripped of his license, but the doubt still lingers in many parents’ minds.
In the United States, many parents still believe in the now-discredited MMR-autism link and refuse to vaccinate their children. Other parents choose not to vaccinate for various reasons like religious or health beliefs. In one instance, a boy whose parents opted not to vaccinate returned home to the U.S. after a trip abroad; no one yet knew he was infected with measles. The boy exposed 839 people to the disease and caused 11 additional cases of measles, all in other unvaccinated children, including one infant who had to be hospitalized.

According to a study published in Pediatrics (2010), the outbreak cost the public sector $10,376 per diagnosed case. The study further showed that the intentional non-vaccination of those infected occurred in students from private schools, public charter schools, and public schools in upper socioeconomic areas (Sugerman et al. 2010).[17]
What about the Flu Vaccine?
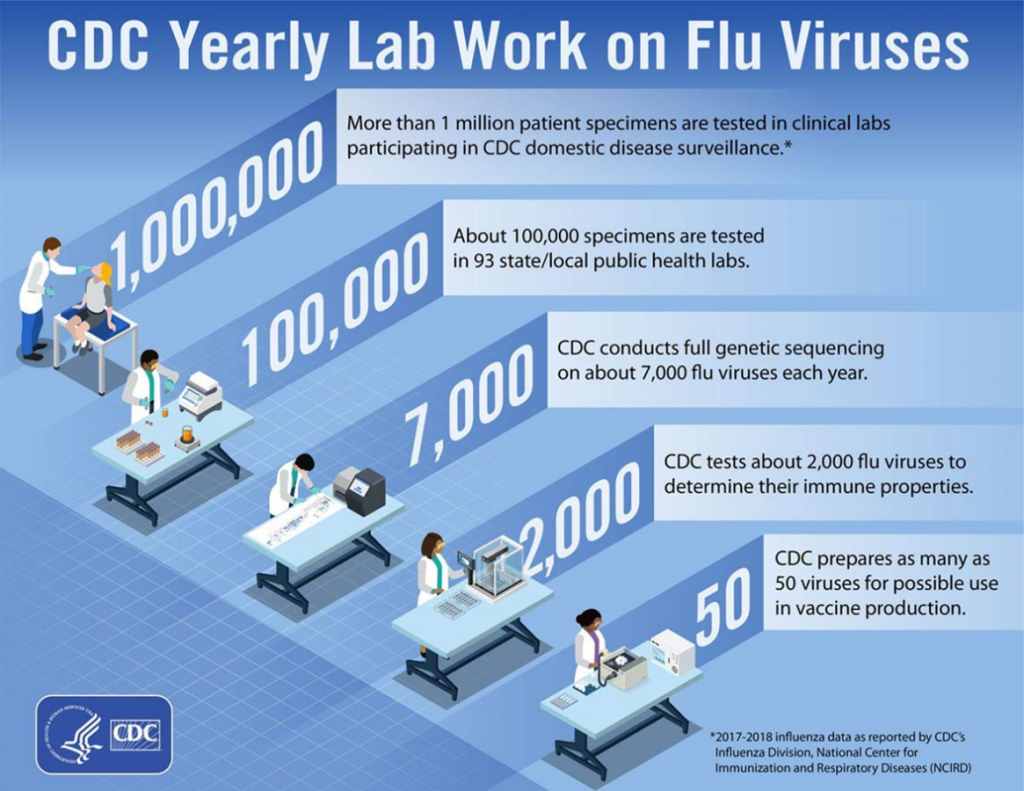
There are many reasons to get an influenza (flu) vaccine each year. Below is a summary of the benefits of flu vaccination, and selected scientific studies that support these benefits.
· Flu vaccination can keep you from getting sick with flu.
· Flu vaccination can reduce the risk of flu-associated hospitalization.
· Flu vaccination is an important preventive tool for people with chronic health conditions.
· Flu vaccination helps protect women during and after pregnancy and helps protect the baby from flu for several months after birth.
· Flu vaccination can be life-saving in children.
· Flu vaccination has been shown in several studies to reduce the severity of illness in people who get vaccinated but still get sick.
· Getting vaccinated yourself may also protect people around you, including those who are more vulnerable to serious flu illness, like babies and young children, older people, and people with certain chronic health conditions.[18]
Pause to Reflect
| Using the information that has been provided about immunizations, think of ways you could respond to the following:
1. “I don’t believe in giving all of the vaccines, like chicken pox. It’s better for children to just get the disease like we all did when we were kids.” 2. “Why do they have to give vaccines so early? It seems like it’s too much, too quickly.” 3. “I have heard that vaccines give some kids autism. And even if they don’t, the side effects are just too scary.” |
Universal Precautions to Prevent the Spread of Illness
There are some standard practices that prevent, or reduce the risk of, the spread of illness in early care and education programs. These are modelled after practices in health care, where everyone is treated as being potentially infected with something that is contagious. Many illnesses are actually contagious before the infected person is symptomatic, so waiting until you see signs of illness is an ineffective way of preventing its spread. Child care providers can practice these four things to help control the spread of illness.
- Hand washing
- Use of disposable nonporous gloves when working with bodily fluids
- Disinfecting potentially contaminated surfaces
- Proper disposal of potentially contaminated waste[20]
Handwashing
Regular handwashing is an important step to minimizing the spread of germs. Hands pick up germs from all of the things they touch and then spread them from one place to another. Germs that are on hands can also enter the body when a person eats or when they touch their eyes, nose, mouth, or any area on the body where the skin is broken (because of a cut, rash, etc.).
All that is needed for handwashing is soap and clean, running water. Handwashing with soap and water removes visible dirt and hidden germs. Studies have demonstrated that handwashing reduced the number of diarrheal illnesses by 31 percent and respiratory illnesses by 21 percent.
Hands should be washed:
- before eating, feeding, or preparing food. This prevents germs from getting into the mouth from hands. (Hygiene practices related specifically to food safety will be addressed in Chapter 15.)
- after touching saliva (after feeding or eating), mucus (wiping a nose, using a tissue), bodily fluids (toileting, diapering), food, or animals
- when visibly dirty, after touching garbage, or after cleaning
The Center for Disease Control recommends the following handwashing steps:
- “Wet your hands with clean, running water (warm or cold) and apply soap.”
- “Rub your hands together to make a lather and scrub your hands well; be sure to scrub the backs of your hands, between your fingers, and under your nails.”
- “Continue rubbing your hands for at least 20 seconds. Need a timer? Hum the “Happy Birthday” song from beginning to end twice.”
- “Rinse your hands well under running water.”
- “Dry your hands using a clean towel or air dry them.”

Infants and young children will need help with handwashing. Caring for Our Children recommends that caregivers:
- Safely cradle an infant in one arm to wash their hands at a sink.
- Provide assistance with handwashing for young children that cannot yet wash their hands independently.
- Offer a stepping stool to young children so they may safely reach the sink.[22]
Wearing Disposable Gloves
Teachers and caregivers should wear gloves when they anticipate coming into contact with any of the following (on a child’s body or a contaminated surface)
- Blood or bodily substances (i.e., fluids or solids)
- Mucous membranes (e.g., nasal, oral, genital area)
- Non-intact skin (e.g., rashes or cuts and scrapes)[23]
Once the gloves are soiled, it’s important to remove them carefully.
- Using a gloved hand, grasp the palm area of the other gloved hand and peel off the first glove.
- Hold the removed glove in the gloved hand.
- Slide the fingers of the ungloved hand under the remaining glove at the wrist and peel off the second glove over the first glove.
- Discard the gloves in a waste container.[24]

After you remove your gloves you should wash your hands. “Do not reuse the gloves: this can spread germs from one child to another…Gloves provide added protection from communicable diseases only if used correctly. If you use gloves incorrectly, you actually risk spreading more germs than if you don’t use gloves at all. Pay attention to your gloving technique so that you do not develop a false sense of security (and carelessness) when wearing gloves.”[26]
Cleaning and Disinfecting
Washing Surfaces Germs spread onto surfaces from hands and objects (tissues or mouthed toys) or from a sneeze or cough. It is important to clean all surfaces well, including toys and any surface that a young child puts in his mouth because germs cannot be seen and it is easy to overlook surfaces that do not look soiled or dirty.
Toileting and diapering involve germs from bodily fluids and fecal material. These germs spread easily in a bathroom onto hands, flushers, and faucets. Routinely washing bathroom surfaces removes most germs and prevents them from spreading. The kitchen is another area of the home where it is important to clean surfaces well.
The terms “cleaning,” “sanitizing,” and “disinfecting” deserve close attention.
Cleaning removes visible soil, dirt, and germs. Soap and water will clean most surfaces.
Sanitizing reduces but does not totally get rid of, germs to a level that is unlikely to cause disease. Sanitizers may be appropriate to use on surfaces where you eat (such as a table or high chair tray) and with toys that children place in their mouths. It is important to follow the instructions on the label, which may also include rinsing surfaces after using the sanitizing product.
Disinfecting destroys or inactivates infectious germs on surfaces. Disinfectants may be used on diaper-changing tables, toilets, and countertops.[27]
Early care and education programs can create a bleach and water solution of one tablespoon of household bleach to one-quart of water for surfaces that need to be sanitized or disinfected. To use effectively, the surface must be wetted with the solution and allowed to air dry. A fresh bleach solution should be made each day to maintain effectiveness, and stored in a clearly labeled spray bottle out of children’s reach. Research shows that other chemicals (e.g., ammonia, vinegar, baking soda, Borax) are not effective against some bacteria.[28] “Items that can be washed in a dishwasher or hot cycle of a washing machine do not have to be disinfected because these machines use water that is hot enough for a long enough period of time to kill most germs.”[29]
Cleaning and disinfecting are essential. Studies have shown that some germs, including influenza virus, can survive on surfaces for two to eight hours; rotavirus can survive up to 10 days.[30]
Table 8.2 – Schedule for Cleaning and Disinfecting[31]
| Surface/Item | Clean | Disinfect | Frequency |
| Countertops and Tabletops | X | X | Daily and when soiled |
| Food prep and service areas | X | X | Before and after use; between prep of raw and cooked food |
| Floors | X | X | Daily and when soiled |
| Door and cabinet handles | X | X | Daily and when soiled |
| Carpets and large rugs | X | Vacuum daily; clean monthly for infants, every 3 months for other ages and when soiled | |
| Small rugs | X | Shake or vacuum daily; launder weekly | |
| Utensils, surfaces, and toys that go in the mouth or have been in contact with bodily fluids | X | X | After each child’s use |
| Toys not contaminated with bodily fluids | X | Weekly | |
| Dress up clothes not worn on the head | X | Weekly | |
| Hats | X | After each child’s use | |
| Sheets and pillowcases | X | Weekly and when visibly soiled | |
| Blankets and sleeping bags | X | Monthly and when visibly soiled | |
| Cubbies | X | Weekly | |
| Cribs | X | Weekly | |
| Handwashing sinks including faucet, soap dispenser, and surrounding area | X | X | Daily or when soiled |
| Toilet seats, handles, door knobs or handles in toileting area, floors | X | X | Daily and immediately is soiled |
| Toilet bowls | X | X | Daily |
| Changing tables | X | X | After each child’s use |
| Potty chairs (discouraged in child care because of contamination risks) | X | X | After each child’s use |
| Any surface contaminated with bodily fluids (saliva, mucus, vomit, urine, stool, or blood) | X | X | Immediately |
| Water containers | X | X | Daily |
Disposal of Waste
Proper disposal and storage of garbage waste prevent the spread of disease, odours, and problems with pests. Disposable items (diapers, gloves, paper towels, and facial tissues) should be thrown away immediately in an appropriate container. Make sure the container is water and rodent-proof, operated with a foot pedal, is lined with a plastic bag, within reach of the diaper-changing area, handwashing sink, and food preparation areas, out of reach of and unable to be knocked over by infants and toddlers. The containers should be emptied, cleaned, and sanitized daily.[32]
Diaper Changing
Diaper changing areas should be smooth and nonporous (such as a plastic-covered pad), have a raised edge to prevent children from falling, be near a sink, be out of reach from children, and be away from food preparation areas.[33]
The following diaper-changing procedure should be posted in the changing area and followed to protect the health and safety of children and staff:
Step 1: Before bringing the child to the diaper changing area, perform hand hygiene (including putting on gloves, if using), bring supplies to the diaper changing area, and place a disposable liner on the changing area.
Step 2: Carry/bring the child to the changing table/surface, keeping soiled clothing away from you and any surfaces you cannot easily clean and sanitize after the change. Always keep a hand on the child.
Step 3: Remove the soiled diaper and clothing without contaminating any surface not already in contact with stool or urine. Put soiled diapers in the lined waste container. Put any soiled clothing in a plastic bag that is securely closed to give to the family.
Step 4: Clean the child’s diaper area with disposable wipes and place soiled wipes into a lined waste container.
Step 5: Removed the disposable liner and gloves and place them in the waste container
Step 6: Use facial tissue to apply any creams or ointments. Slide a clean diaper under the child fasten it and dress the child.
Step 6: Wash the child’s hands and return the child to a supervised area.
Step 7: Clean and disinfect the diaper-changing surface and any equipment or supplies that were touched (and any other area the child soiled before changed).
Step 8: Perform hand hygiene and record the diaper change, diaper contents, and/or any problems.
Caregivers/teachers should never leave a child unattended on a table or countertop. A safety strap or harness should not be used on the diaper changing table/surface.[34]
If Using Potty Chairs
Due to being hard to clean and disinfect, potty chairs are not ideal in a child care environment. If they are used, they should be used in the bathroom only. After each use:
· Empty contents immediately into the toilet
· Rinse with water and dump water into the toilet
· Wash with soap and water (with a paper towel) and empty soapy water into the toilet
· Rinse again and empty into the toilet
· Spray with bleach solution
· Air dry
· Wash and disinfect the sink.
· Wash hands (child and adult)[35]
Pause to Reflect
| You are at a job interview to become a teacher in an infant room and the director asks you what you would do to prevent the spread of illness in your classroom. What might you want to mention? |
Children’s Environmental Health
Environmental Exposures and Children’s Vulnerability
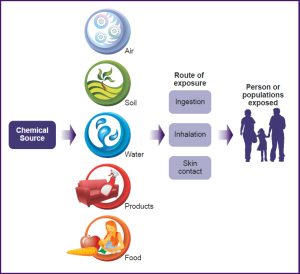
We live in a world in which we are surrounded by chemicals (natural and human-made) and those chemicals can have a detrimental effect on our health. Environmental health looks at how chemicals in our environment have an impact on our well-being. To understand environmental health in children we must first look at where the chemicals come from and how they enter our bodies. As the image below illustrates chemicals can come from the air, water, soil, products, and the food we eat. They can enter our bodies through three (3) routes of exposure – ingestion, inhalation and skin contact.
Sometimes the threat to health comes from the environment itself. Air quality, chemical hazards, drinking water, mould, and pest management are all topics that early care and education providers should be aware of.
So, what does this have to do with ECE? As educators, we need to understand how chemicals and environmental toxins affect children so that we can take the needed steps to protect them from harm.
“Environmental exposures start in the womb and can have effects throughout life. The prenatal and early childhood period represents a window of particular vulnerability, where environmental hazards can lead to premature birth and other complications. Early childhood exposure to such hazards can also increase lifelong disease risk including for respiratory disorders, cardiovascular disease and cancers…” [37]
| “Environmental exposures start in the womb and can have effects throughout life. The prenatal and early childhood period represents a window of particular vulnerability, where environmental hazards can lead to premature birth and other complications. Early childhood exposure to such hazards can also increase lifelong disease risk including for respiratory disorders, cardiovascular disease and cancers…” [38] |
Now that we understand where toxins and chemicals are found and how they enter our bodies, the next important thing we need to understand is that adults and children are different when it comes to exposure to chemicals and toxins.
As early childhood educators, we know that children are not “mini-me”. You know, although children look like “small adults” they are not! Due to their rapid development, children are more vulnerable than adults to environmental toxins/chemicals. (Footnote
| “The rapid development of a child’s organ systems during embryonic, fetal, and early newborn periods makes the young more vulnerable when exposed to environmental toxicants.”[39] |
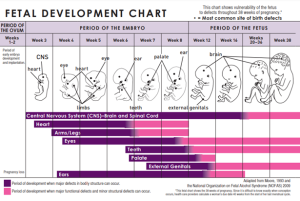
As discussed in the video above children have windows of vulnerability where they are more vulnerable at specific times during human development that have been identified as higher risks to health. An example is during fetal development – see the chart below [41]. It shows the development of a fetus and highlights the times when the development of specific “bodily structures” are more at risk or susceptible to damage by environmental toxins.
As early childhood educators, you must understand the concern for the environmental health of children. Although low levels of exposure to a toxin or chemical, for an adult may be okay in the short term, this is not always the case for a child.
Children may look like “small adults” but as we know this is not the case and in terms of environmental health it is important to understand the difference.
Children are Different! They are not small adult and because of that, they are more vulnerable to toxins than adults are. There are four distinct ways that adults and children differ which leads to children being more a risk in environments that they share with adults.
There are four ways that children differ from adults in relation to children’s increased vulnerability to environmental toxins and they are proportionality, behaviour, physiology and life expectancy/Latency.
Proportionality
As stated earlier, children’s size compared to that of an adult is different. Not just in basic size, but more importantly in their proportions. It is these differences in proportions that are key to understanding why children are more vulnerable to environmental toxins and chemicals. [43]
- Lung size or the surface area of children’s lungs is larger than that of adults [44]. Due to this difference in proportion children breathe faster. In addition to their “at rest” or basal breathing being faster than that of adult, they are also more likely to speed up their breathing due to their increased activity level. As a result of breathing faster or more often than adults, children breathe in toxins at an accelerated – making them more vulnerable.
- “Kilogram for Kilogram of body weight” a child will eat more food and drink more water than that of an adult. For example: if both a child and an adult ate a banana and drank a glass of water the contamination level in the banana and water would be higher for the child than the adult due to the difference in their proportions. [45]
- Children’s brains are also proportionally larger than adults and receive twice the blood flow than adults [46]
Behaviour
- Children are not only closer to the ground than adults, but they also spend most of their time there – both indoors and outdoors. More vapours and dust can be found on the ground in higher concentration and are in the direct vicinity of a child’s breathing zone [47]
- Infants crawl around on the ground, and they explore their world with their hands and mouth – adults tend not to as much. Again, being close to the ground and exploring things that have fallen on the ground with their mouths make them more vulnerable.
Physiology
- Due to their rapid biological development, children also have a greater metabolic need for oxygen – leading to faster breathing rates.
- Children’s nervous system, respiratory system, reproductive system, and digestive system are still developing which makes them more vulnerable to toxins.
- As children develop so does the rate of absorption, distribution, storage, metabolism, and excretion of chemicals. Depending on the child’s developmental stage exposure to toxins has varying effects, unlike adults who are less vulnerable to toxins.
| “Metabolism is the combined package of all the life-sustaining chemical processes occurring in any living organism. Children tend to have a faster metabolism than do adults. They need to take in more oxygen per unit of body weight per minute to support their growth and activity needs, which are driven by their higher metabolic rates” [48] |
Live expectancy or Latency
- The latency period is the “…period of time between exposure to a disease-causing agent and the first appearance of signs or symptoms of the disease” [49]. For example: If a child and an adult are exposed to a toxin that causes cancer in adulthood, at the same moment in time – a child is more at risk because he will live more years with the effect of that exposure than an adult will. Children are also still developing, and that exposure affects a child differently than a fully developed adult.
| “The environment in which children grow, play and learn has a profound effect on their health and well-being. Exposures to a polluted indoor environment do not result in the same outcomes for children as for adults because children may be exposed differently, children metabolize some chemicals differently than adults; and children have “windows of vulnerability” while they are growing and developing when their target organs may be more susceptible than the target organs of adults” [50]. |
Outdoor Air Quality
Children are more susceptible to the effects of contaminated air because they breathe in more oxygen relative to their body weight than adults.[51] Therefore, they “can be exposed to a lot of pollution. Children should be kept inside when air quality is poor, or should at least be discouraged from intense outdoor activity. Educators and parents should be aware that nearby construction and traffic can increase pollution. Mowing school lawns should never occur during school hours since this can cause an allergy or asthma attack. Insecticides should never be sprayed while children are in care. Outdoor air can include odours, pollutants from vehicles, and fumes from stored trash, chemicals, and plumbing vents.”[52]
Indoor Air Quality
There are so many sources of indoor air pollution in childcare facilities that the air is considered to be two to five times more polluted than outdoor air. Common sources of indoor air pollution include combustion sources such as oil, gas, kerosene, coal, wood, and tobacco products; building materials and furnishings as diverse as deteriorated, asbestos-containing insulation, wet or damp carpet, and cabinetry or furniture made of certain pressed wood products; products for household cleaning and maintenance, personal care, or hobbies; central heating and cooling systems and humidification devices; and outdoor sources such as radon, pesticides, and outdoor air pollution.[53]
Key Takeaways
Environmental Tobacco Smoke & Dangers of E-Cigarettes

Environmental tobacco smoke (ETS), otherwise known as secondhand smoke, is a mixture of the smoke given off by the burning end of a cigarette, or cigar, and the smoke exhaled by smokers. Secondhand smoke contains more than 4,000 substances, several of which are known to cause cancer. Children are particularly vulnerable to the effects of secondhand smoke because they are still developing physically, have higher breathing rates than adults, and have little control over their environment, including where and when the adults in their world choose to smoke. Exposure to secondhand smoke can cause asthma, and places infants and children at increased risk for Sudden Infant Death Syndrome (SIDS), pneumonia, bronchitis, and middle ear infections.[55]

Scientists are still working to understand more fully the health effects and harmful doses of e-cigarette contents when they are heated and turned into an aerosol, both for active users who inhale from a device and for those who are exposed to the aerosol secondhand. Another risk to consider involves defective e-cigarette batteries that have been known to cause fires and explosions, some of which have resulted in serious injuries. Most of the explosions happened when the e-cigarette batteries were being charged.[57]
Mould
Mould is a fungus that thrives indoors when excessive moisture or water accumulates indoors or when moisture problems remain undiscovered or unaddressed. There are moulds that can grow on wood, paper, carpet, and foods. There is no practical way to eliminate all mould and mould spores in the indoor environment. The way to control indoor mould growth is to control moisture.
Mould needs to be controlled in childcare settings to avoid possible health impacts for infants and children, including allergic reactions, asthma, and other respiratory issues.[58]
Integrated Pest Management
Exposure to pests such as cockroaches, rodents, ants, and stinging insects in childcare centers may place children at risk for disease, asthma attacks, bites, and stings. Improper use of pesticides can also place children at risk. A recent study of pesticide use in child care centers revealed that 75% of centers reported at least one pesticide application in the last year. Several factors increase both children’s exposure and their vulnerability to these exposures compared to adults. Children spend more time on the floor, where residues can transfer to the skin and be absorbed.
Young children also frequently place their hands and objects in their mouths, resulting in the non-dietary ingestion of pesticides. Children are less developed immunologically, physiologically, and neurologically, and therefore may be more susceptible to the adverse effects of chemicals and toxins. There is increasing evidence of adverse effects of pesticides on young children, particularly on neurodevelopment.[59]
Integrated Pest Management (IPM) is an effective and environmentally sensitive approach to pest management that relies on a combination of common-sense practices. IPM programs use current, comprehensive information on the life cycles of pests and their interaction with the environment.
Integrated Pest Management “(IPM) is a safer, more effective, longer-lasting method of pest control that emphasizes pest prevention by eliminating pests’ access to food, water, and shelter. When using IPM, properly identify the pest and know why it’s there so an appropriate combination of different pest control methods can be used for better effectiveness in controlling the pest.”[60] This information, in combination with the last toxic available pest control methods, is used to manage pest damage by the most economical means, and with the least possible hazard to people, property, and the environment.[61]

Chemical Hazards
A child born today will grow up exposed to more chemicals than a child from any other generation in our nation’s history. Of the 85,000 synthetic chemicals in commerce today, only a small fraction has been tested for toxicity to human health.
A 2005 study found 287 different chemicals in the cord blood of 10 newborn babies – chemicals from pesticides, fast food packaging, coals, gasoline emissions, and trash incineration. Children are more vulnerable to toxic chemicals because their bodies are still growing and developing.[63]
Plastics in Child Care Settings
Certain types of plastics contain chemicals such as phthalates, bisphenol A (BPA), polyvinyl chloride (PVC), and polystyrene that can be toxic to children. These plastics could be found in baby bottles, sippy cups, teething rings, pacifiers, and toys. When these items are in a child’s mouth or when they are heated (such as in a microwave), children can be exposed to harmful chemicals that have the potential to mimic or suppress hormones and disrupt normal growth and development.[64]
In 2009 Canada was the country to declare that BPA was a ‘dangerous substance’. This declaration led to the prohibition of BPA in the Canadian Consumer Products Act. Section 5 states “No person shall manufacture, import, advertise or sell a consumer product listed in Schedule 2”

Drinking Water
Canada has one of the safest public drinking water supplies in the world. Water management is shared by Federal, Provincial and Municipal governments.
Sources of drinking water are subject to contamination and require appropriate treatment to remove disease-causing contaminants. Contamination of drinking water supplies can occur in the source water as well as in the distribution system after water treatment has already occurred. There are many sources of water contamination, including naturally occurring chemicals and minerals (for example, arsenic, radon, uranium), local land use practices (fertilizers, pesticides, concentrated feeding operations), manufacturing processes, and sewer overflows or wastewater releases.
The presence of contaminants in water can lead to adverse health effects, including gastrointestinal illness, reproductive problems, and neurological disorders.[65] Young children are at particular risk for exposure to contaminants in drinking water because, pound for pound, they drink more water than adults (including water used to prepare formula), and because their immature body systems are less efficient at detoxification. Exposure to lead in drinking water is a serious health concern, especially for young children and infants since elevated lead levels in children may result in delays in physical or mental development, lower IQ, and even brain damage.[66]

Pause to Reflect
| What are five important things that early care and education programs should remember about environmental health to keep children healthy? |
Engaging Families
Teachers can use the following strategies to help families to develop their children’s health habits:
· Provide families with concise, accurate information about ways to promote and develop good health habits in children; information should be presented in English and the families’ home languages. Capture their interest by addressing topics related to their children’s age and development, as well as topics related to common health risks for children, such as childhood obesity, asthma, and dental caries. Injury prevention and first-aid topics, such as treating burns, bleeding, and choking, are also relevant. Provide written informational materials that are brief and easy to read.
· Provide individualized information, as well as general health information, to all families through daily contact, workshops, and parent meetings. All information should be presented in English and in the families’ home languages. Accommodate family schedules by providing workshops and meetings at various times (e.g., morning, afternoon, evening), and arrange for child care during meetings.
· Show family members what the children are learning by sending home examples of work, encouraging families to visit the preschool and observe children in action, and sharing children’s portfolios during home visits. Reinforce children’s learning about health habits through take-home activities, lending libraries of read-aloud books in the languages of the families in the group, and displays of children’s work.
· As you introduce health routines (e.g., handwashing, tooth brushing), invite family members to participate and model. Encourage families to contribute ideas or materials to interest areas that reflect diverse health habits at home.
· Identify community resources related to health habits (e.g., handwashing, tooth brushing) and invite community personnel to participate in and bring resources to family workshops or parent meetings. Emphasize the role of home and family members in helping children to develop health habits, and inform all parents of the availability of free and low-cost community resources.
· Be sensitive to and respectful of different values or beliefs, as well as varying levels of access to health products and services. Gather information on available and accessible resources in the community, including those for children with special needs, and provide this information to all families, translated into their home languages.
Summary
Understanding how illness is spread, helps early care and education programs prevent the spread of illness. Immunizations also play an important role in preventing illness. And when program staff use universal precautions, including handwashing, cleaning and disinfecting, and proper disposal of waste, they also prevent the spread of illness.
Programs must also be aware of environmental hazards that present a threat to children’s health. These include both indoor and outdoor air quality, mould, and chemicals. Programs should use integrated pest management and make sure that their drinking water is safe as well.
Resources for Further Exploration
Health and Safety in the Child Care Setting: Prevention of Infectious Disease A Curriculum for the Training of Child Care Providers (3rd edition): https://cchp.ucsf.edu/sites/g/files/tkssra181/f/PHT-Handbook-Student-2018-FINAL.pdf
Safe and Healthy Child Care Centers: https://www.epa.gov/sites/production/files/documents/SafeHealthy2012_ENGa.pdf
Handwashing: https://www.cdc.gov/handwashing/index.html
Vaccines: https://www.cdc.gov/vaccines/
Environmental Health in Child Care: https://www.epa.gov/childcare
California Childcare Health Program’s Publications and Resources: https://cchp.ucsf.edu/content/resources
Air Quality: https://legacy.azdeq.gov/function/about/download/indoorair.pdf
Mold Remediation in Schools: https://www.epa.gov/mold/mold-remediation-schools-and-commercial-buildings-guide
Integrated Pest Management in Child Care Centers: https://www.epa.gov/sites/production/files/documents/IPM_CCC.pdf
California School & Child Care Integrated Pest Management (IPM): https://apps.cdpr.ca.gov/schoolipm/
Healthy Schools Act Compliance Packet for Childcare Centers: https://apps.cdpr.ca.gov/schoolipm/school_ipm_law/hsa_compliance_childcare_packet.pdf
EPA’s 3TsWater Quality Tool Kit: https://www.epa.gov/ground-water-and-drinking-water/3ts-reducing-lead-drinking-water-toolkit
References
- Image by College of the Canyons ZTC Team is based on image from Managing Infectious Disease in Head Start Webinar by Head Start Early Childhood Learning & Knowledge Center, which is in the public domain ↵
- Image from Managing Infectious Disease in Head Start Webinar by Head Start Early Childhood Learning & Knowledge Center is in the public domain ↵
- Image by College of the Canyons ZTC Team is based on Image by the CDC Division of Vector-Borne Diseases, which is in the public domain ↵
- Managing Infectious Disease in Head Start Webinar (Transcript) by Head Start Early Childhood Learning & Knowledge Center is in the public domain ↵
- How does disease spread?, CDC NERD Academy, CDC ↵
- Managing Infectious Disease in Head Start Webinar (Transcript) by Head Start Early Childhood Learning & Knowledge Center is in the public domain ↵
- For Parents: Vaccines for Your Children by the CDC is in the public domain ↵
- Sourced from image by the CDC is in the public domain ↵
- Disease Prevention and Healthy Lifestyles references Contemporary Health Issues by Judy Baker, Ph.D., licensed under CC BY-SA 4.0 ↵
- Making the Vaccine Decision by the CDC is in the public domain ↵
- Image by the CDC is in the public domain ↵
- Disease Prevention and Healthy Lifestyles references Contemporary Health Issues by Judy Baker, Ph.D., licensed under CC BY-SA 4.0 ↵
- Making the Vaccine Decision by the CDC is in the public domain ↵
- Disease Prevention and Healthy Lifestyles references Contemporary Health Issues by Judy Baker, Ph.D., licensed under CC BY-SA 4.0 ↵
- Making the Vaccine Decision by the CDC is in the public domain ↵
- [17] Image by CDC Global is licensed under CC BY 2.0 ↵
- Disease Prevention and Healthy Lifestyles references Contemporary Health Issues by Judy Baker, Ph.D., licensed under CC BY-SA 4.0 ↵
- What Are the Benefits of Flu Vaccination? by the Centers for Disease Control and Prevention is in the public domain ↵
- Image by the Centers for Disease Control and Prevention is in the public domain ↵
- California Child Care Health Program. (2011). Health and Safety in the Child Care Setting: Prevention of Infectious Disease. University of California San Francisco. https://cchp.ucsf.edu/sites/g/files/tkssra181/f/idc2book.pdf ↵
- Stop Germs! Wash Your Hands by the Centers for Disease Control and Prevention is in the public domain ↵
- Health Tips for Home Visitors to Prevent the Spread of Illness by Head Start National Center on Health is in the public domain ↵
- The Basics of Standard Precautions by Karen Jones, Linda R. Greene, and Lona Mody is in the public domain ↵
- Sequence for Putting On Personal Protective Equipment (PPE) by the Centers for Disease Control and Prevention is in the public domain ↵
- Image by the Centers for Disease Control and Prevention is in the public domain ↵
- California Child Care Health Program. (2011). Health and Safety in the Child Care Setting: Prevention of Infectious Disease. University of California San Francisco. Retrieved from https://cchp.ucsf.edu/sites/g/files/tkssra181/f/idc2book.pdf ↵
- Health Tips for Home Visitors to Prevent the Spread of Illness by Head Start National Center on Health is in the public domain ↵
- California Preschool Curriculum Framework (Volume 2) by the California Department of Education is used with permission ↵
- California Child Care Health Program. (2011). Health and Safety in the Child Care Setting: Prevention of Infectious Disease. University of California San Francisco. Retrieved from https://cchp.ucsf.edu/sites/g/files/tkssra181/f/idc2book.pdf ↵
- California Preschool Curriculum Framework (Volume 2) by the California Department of Education is used with permission ↵
- California Child Care Health Program. (2011). Health and Safety in the Child Care Setting: Prevention of Infectious Disease. University of California San Francisco. Retrieved from https://cchp.ucsf.edu/sites/g/files/tkssra181/f/idc2book.pdf ↵
- California Child Care Health Program. (2011). Health and Safety in the Child Care Setting: Prevention of Infectious Disease. University of California San Francisco. Retrieved from https://cchp.ucsf.edu/sites/g/files/tkssra181/f/idc2book.pdf ↵
- California Child Care Health Program. (2011). Health and Safety in the Child Care Setting: Prevention of Infectious Disease. University of California San Francisco. Retrieved from https://cchp.ucsf.edu/sites/g/files/tkssra181/f/idc2book.pdf ↵
- Diaper Changing Procedure by Head Start Early Childhood Learning & Knowledge Center is in the public domain ↵
- California Child Care Health Program. (2011). Health and Safety in the Child Care Setting: Prevention of Infectious Disease. University of California San Francisco. Retrieved from https://cchp.ucsf.edu/sites/g/files/tkssra181/f/idc2book.pdf ↵
- Biomonitoring Image by Government of Canada is in the public domain ↵
- Children’s environmental health Inheriting a sustainable world (factsheet), (2017), by WHO, BY-NC-SA 4.0 ↵
- Children’s environmental health Inheriting a sustainable world (factsheet), (2017), by WHO, BY-NC-SA 4.0 ↵
- ATSDR Case Studies in Environmental Medicine: Principles of Pediatric Environmental Health, (2012), by the U.S. Department of Health and Human Services, in the public domain. ↵
- Video: Protecting Children’s Environmental Health, (2023) by United States Environmental Protection Agency (EPA) ↵
- Image Fetal Development Chart, (2009) by CDC.gov, in the public domain. ↵
- Image Fetal Development Chart, (2009) by CDC.gov, in the public domain. ↵
- Child Health and Environment – A Primer, (2005), by Canadian Partnership for Children’s Health and Environment (CPCHE) ↵
- Child Health and Environment – A Primer, (2005), by Canadian Partnership for Children’s Health and Environment (CPCHE) ↵
- Child Health and Environment – A Primer, (2005), by Canadian Partnership for Children’s Health and Environment (CPCHE) ↵
- Child Health and Environment – A Primer, (2005), by Canadian Partnership for Children’s Health and Environment (CPCHE) ↵
- Child Health and Environment – A Primer, (2005), by Canadian Partnership for Children’s Health and Environment (CPCHE) ↵
- Child Health and Environment – A Primer, (2005), by Canadian Partnership for Children’s Health and Environment (CPCHE) ↵
- Child Health and Environment – A Primer, (2005), by Canadian Partnership for Children’s Health and Environment (CPCHE) ↵
- Ruth A Etzel, (2020) The Special Vulnerability of Children, found in the International Journal of Hygiene and Environmental health, used with Elsevier Open Access CC-BY-NC-ND. ↵
- Resources about Indoor Air Quality for Child Care Providers by the U.S. Environmental Protection Agency is in the public domain ↵
- Indoor Air Quality Issues for Child Care Facilities by the Arizona Department of Environmental Quality is in the public domain ↵
- Resources about Indoor Air Quality for Child Care Providers by the U.S. Environmental Protection Agency is in the public domain ↵
- Image by the U.S. Environmental Protection Agency is in the public domain ↵
- Resources about Environmental Tobacco Smoke for Child Care Providers by the U.S. Environmental Protection Agency is in the public domain ↵
- Image by lindsayfox on Pixabay ↵
- Know the Risks: E-Cigarettes and Young People by the U.S. Department of Health and Human Services is in the public domain ↵
- Resources about Mold for Child Care Providers by the U.S. Environmental Protection Agency is in the public domain ↵
- Resources about Pesticides and Integrated Pest Management for Child Care Providers by the U.S. Environmental Protection Agency is in the public domain ↵
- PennState Extension. (2011, October 11). IPM for Child Care and Early Learning Environments. PennState Extension. Retrieved from https://extension.psu.edu/ipm-for-child-care-and-early-learning-environments ↵
- Integrated Pest Management (IPM) Principles by the U.S. Environmental Protection Agency is in the public domain ↵
- Image by the U.S. Environmental Protection Agency is in the public domain ↵
- Resources about Chemical Hazards for Child Care Providers by the U.S. Environmental Protection Agency is in the public domain ↵
- Resources about Plastics in Child Care Settings for Parents and Providers by the U.S. Environmental Protection Agency is in the public domain ↵
- Water-related Diseases and Contaminants in Public Water Systems by the Centers for Disease Control and Prevention is in the public domain ↵
- Resources about Drinking Water for Child Care Providers by the U.S. Environmental Protection Agency is in the public domain ↵
- Image by Amanda Mills is in the public domain. ↵

